The stages of psoriasis are defined time intervals during which the disease takes on its characteristic features. Many psoriasis mistakenly call stage a severe or mild form of the disease, but in medical records the term is used in a completely different meaning.
What are the stages of psoriasis?

Psoriasis is recognized as a recurrent skin disease, the cause of which is genetics. According to dermatologists, at least 2% of the world population suffers from this disease, which means that the problem is very urgent. During psoriasis, 2 conditions are clearly distinguished:
- Relapse.This term refers to the deterioration of the skin. In case of relapse, the patient suffers from itching, pain, burning, abundant rashes, irritation and discomfort. The victim's situation is aggravated by insomnia, neurosis and anxiety.
- Remission.This word is used to indicate improvement in the appearance of the skin. With remission, the skin regains its normal color, the redness disappears and the area of the psoriatic plaques is reduced.
The stages of psoriasis partly duplicate the description of remissions and relapses, so many dermatologists use these words interchangeably. In clinical practice, 3 stages of psoriasis are described:
- progress phase;
- stationary;
- regression phase.
Considering that we are talking about a cyclic process, the phases sequentially flow into each other and form a continuous course of the disease.
Done!The progress phase is considered the hardest to hear.
What is the progress of psoriasis?
The progress phase is triggered by a number of triggers, such as cold weather or stress. In some cases, even an experienced dermatologist cannot unambiguously determine the trigger. During the progressive phase, the following happens:

- Psoriatic nodules develop rapidly, affect the skin, interconnect in so-called plaques, which flake and itch. A plaque is a point of arbitrary shape, most often round or oval, sometimes with an irregular edge.
- Papules, that is, the individual nodules of a psoriatic rash, are lumps on the skin. The edges of the papules do not break off and the central part is detached. When a large number of dead scales accumulate, the plaques begin to rise above the surface of the skin. The swelling gives them an even more convex and uneven appearance.
- This stage of the pathology is characterized by an isomorphic reaction, which consists in the exacerbation of rashes in case of skin lesions, scratches, injections, cuts, microtraumas. This phenomenon bears the name of Köbner.
A delayed reaction is characteristic of the progressive stage of psoriasis. In some cases, rashes appear about 9 days after exposure to a trigger (such as a food allergen). Typically, a psoriatic rash appears within 24 hours of exposure to adverse factors.
Interesting!95% of psoriasis have some kind of food intolerance that can trigger a relapse. To avoid exacerbations, it is necessary to keep a food diary and observe the reaction to different types of food.
Stationary and recessive stages
The stationary stage is the period in the course of psoriasis during which the victim's condition is relatively stabilized. In the stationary phase:

- Psoriatic plaques have a smooth outline. The entire surface of the plate is covered with a thick layer of scales that peel off easily. Itching and discomfort are moderate. There is no bright red inflamed border around the papules.
- With microtraumas of the skin, Koebner's phenomenon is not observed, i. e. scratching or cutting healthy skin no longer turns into a psoriatic plaque.
The regressive or recessive phase is characterized by massive lesions in psoriasis. First, a pseudo-atrophic border can be seen around the papules, then patients notice a rapid cessation of skin peeling, with the formation of hyperpigmentation plaques at the site.
Pathological severity
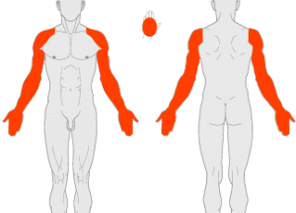
A further diagnostic criterion is the evaluation of the area of psoriatic lesions. The term "gravity" is used to describe it. Dermatologists distinguish 3 degrees of severity of the skin disease:
- Easy.Psoriatic plaques occupy 1 to 3% of the total body surface. The small size of the affected areas does not mean that the patient is well. With psoriasis of the head or face, even a couple of plaques will be enough to cause a person discomfort and distress.
- Medium.The volume of psoriatic eruptions occupies 3 to 10% of the total body surface. In this case, the back, chest and outer surfaces of the joints, scalp, palms and feet are affected. This prevalence leads to severe intoxication and severe pain. The patient may completely or partially lose his ability to work, the mental state and the state of the nervous system deteriorate.
- Heavy.The disease covers more than 10-15% of the skin surface. According to rough estimates, if psoriasis occupies more than a quarter of the total body surface, the likelihood of liver or kidney failure increases many times. Decompensated damage to internal organs can cause psoriasis to die.
To fully assess the severity of psoriasis, a special scale called PASI is used. The scale takes into account:
- percentage of healthy and diseased skin;
- stage of the pathology;
- patient response to drug therapy;
- individual tolerance of psoriasis (mental state, complications of the nervous system and psyche);
- objective data of laboratory tests in dynamics (for example, the volume of uric acid in a blood test).
The diagnosis takes into account all the symptoms that affect the condition of a person with psoriasis. The intensity is reflected in the medical record:
- itchy skin processes;
- redness;
- swelling;
- hyperemia;
- thickening of the skin;
- exfoliation;
- blood flow;
- swelling;
- infections;
- pain syndrome.
On the PASI scale, the volume of skin lesions is described by numbers, from 0 to 72, where 0 is the absence of skin symptoms and 72 is the large-scale and maximum possible spread of the disease.
Attention!It is important that the patient first of all knows and checks for signs of exacerbation. If unfavorable symptoms appear, you should immediately visit a dermatologist, because psoriasis does not always go into the stationary phase itself. A relapse can last for decades.
Treatment of psoriasis depends on the stage
For each stage of the disease, its own set of therapeutic measures have been developed, so the first thing a dermatologist determines is whether psoriasis is progressing, stabilizing or regressing.
How the progressive phase is treated
Every psoriasis sufferer assumes that remission is coming to an end from their feelings. If the itching is getting worse, the skin is getting worse and the psoriasis is clearly spreading over the surface of the body, treatment should be started. The therapy for the advanced stage has the following characteristics:
- The patient is engaged in the prevention of further deterioration, strictly adheres to the diet, refrains from the triggers of the pathological process (stress, smoking, alcohol).
- For severe itching, antihistamines can be used, an additional benefit of this class of drugs is the removal of swelling in the area of psoriatic plaques.
- A dermatologist prescribes a wide range of topical treatments to heal, soften and thin the skin. By decision of the doctor, creams, ointments or sprays are selected. Tar soap and solid oil compresses give positive dynamics. You can also apply compresses or apply cosmetics with Dead Sea mud.
The main task at this stage is to stop the exacerbation before the disease enters a prolonged relapse. According to the indications, the doctor selects corticosteroids injections or in the form of ointments.
Attention!Corticosteroids should be used in a short, intensive course under the supervision of a dermatologist. You can give yourself injections or spread antihistamine ointments.
Stationary and regressive therapy

Further actions of the dermatologist depend on the body's response to the selected treatment. The following scenarios are possible:
- Medicines have a positive effect. Within 1-2 weeks, psoriasis passes the stationary phase, regresses and remission occurs.
- Medicines have no effect. If, after 2-4 weeks from the moment of prescribing the course of drugs, the results are still not visible, this is a reason to change the list of drugs or the attending physician.
- Drugs aggravate. This dynamic is also possible, especially if the dose or frequency of administration is not sufficient. Relapse is delayed, psoriatic plaques cover a large area of the body, the person needs hospitalization.
In a medical institution, a more powerful therapy is used, for example, blood purification by hardware. With a favorable reaction, psoriasis enters the stationary phase, which can last from several days to several months.
Interesting!More than 80% of patients note the seasonal nature of the exacerbations. This makes the disease predictable and allows you to prepare for the onset of relapse.
The drug list for the stationary and regressive phase is exactly the same, but the dosage and frequency of administration are lower than in the progressive phase.
10-15 year remission
A competent dermatologist sets himself the following task: to choose such drugs and physiotherapeutic agents that will give psoriasis the most lasting improvement. In this case, the patient himself should do his best to promote treatment, avoid triggers, and take medications responsibly. If the alliance between the patient and the doctor has developed successfully, the duration of remission is unlimited. Stable well-being can last 15 years or more.
























